A System that heals
Context
During the Covid-19 pandemic, the overcrowding of hospitals with anxious patients, the stress on families, desperate for credible advice, brought to the fore the need for family doctors and a resilient primary health system.
Background
- Primary healthcare is defined as “a whole-of-society approach to health and well-being centered on the needs and preferences of individuals, families, and communities.”
- However, the pandemic of novel coronavirus showed the fragility of the existing healthcare delivery system of India.
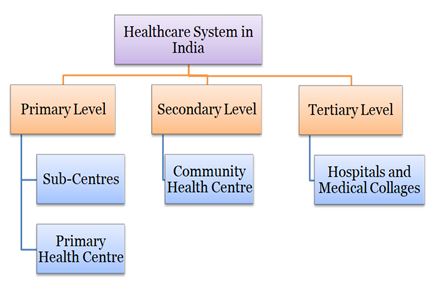
- In India, primary care infrastructure exists as a network of sub-centres, primary health centres and community health centres.
|
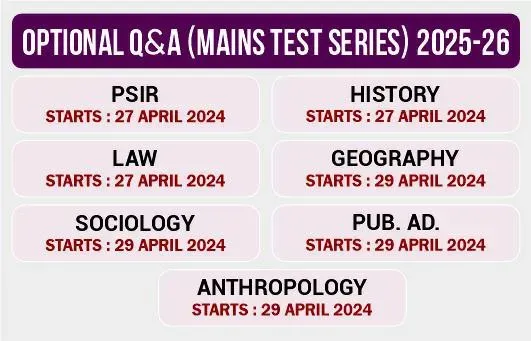
Important Government Policies
|
- However, the focus of services has remained narrow, largely prioritized around reproductive, maternal and child healthcare, and some communicable diseases (notably, malaria).
- The National Health Policy (NHP), 2017, envisages comprehensive primary health care delivered through health and wellness centres (HWCs).
- The policy also commits that two-thirds or more of government spending will be targeted at primary care.
- Additionally, the announcement of Ayushman Bharat by the government is a game changer.
Therefore, this brief aims to highlightthe current status of primary healthcare services in the country and also suggests certain appropriate measures that can be implemented to make the system effective.
Analysis
Why PHC matters?
- Betterment of nation: Primary health care is a key enabler for higher life expectancy, better health outcomes and lower costs for the nation.
- Reducing the burden on other segments: Primary health interventions help detect diseases early, well before complications set in, thus pre-empting the need for secondary and tertiary care.
- Universal Health Coverage: For universal health coverage (UHC) to be truly universal, a shift is needed from health systems designed around diseases and institutions towards health systems designed for people, with people.
- Achievement of health related Sustainable Development Goals (SDGs) and health security.
|
The number game: In the Economic Survey of 2022, India's public expenditure on healthcare stood at 2.1% of GDP in 2021-22 against 1.8% in 2020-21 and 1.3% in 2019-20. |
Why India’s healthcare system is struggling (constraints)?
- Limited scope: The existing primary health care model in the country is limited in scope. Even where there is a well-functioning public primary health centre, only services related to pregnancy care, limited childcare and certain services related to national health programmes are provided, which represent only 15 per cent of all morbidities for which people seek care.
- Implementation issues:The conversion of 150,000 sub centres into HWCs was announced in the budget speech in 2017 and was enshrined in the NHP, 2017.
- Although less than 4000 such centres were sanctioned in 2017-18, the government is committed to accelerating the pace of sanctioning and putting up HWCs to meet the target in good time.
- Inadequate quality: Supply side deficiencies, poor management skills and lack of appropriate training and supportive supervision for health workers prevent delivery of the desired quality of health services.
- Ignored urban population: A primary health care model for the growing urban population has not been conceptualized, notwithstanding a few assorted initiatives by some states.
- Lack of participation/awareness: Although the National Health Mission focuses on engaging communities through village health, nutrition and sanitation societies, health has not yet become a people’s movement.
- Lack of funding: Funding for health is inadequate, leading to low spending on primary care.
|
Developed nations such as the UK, Australia, Canada, Netherlands and Sweden spend a large share of their federal healthcare budgets on primary care. |
- High rate of expenditure:Citizens have to incur high out-of-pocket expenditure on primary health care, of which the largest expenditure is on drugs.
- Other major issues include:
- low number of institutions
- shortage of adequately trained and motivated personnel
What measures are required now?
Accelerate the establishment of a network of 150,000 HWCs
- Ensuring sufficient coverage: Operationalize a network of 150,000 HWCs on priority by 2022-23 in order to ensure sufficient coverage of affordable primary care and lower the burden on secondary and tertiary care.
- Focusing on facilities: HWCs should provide services such as screening and management of non-communicable diseases; screening and basic management of mental health ailments; care for common ophthalmic and ENT problems; basic dental health care; geriatric and palliative health care, and trauma care and emergency care.
- The key features of New India’s primary health care system will be:
- A primary health care nucleus comprising five to six upgraded sub-centres coupled with a primary health centre, and population outreach.
- A team led by a mid-level health service provider,3 auxiliary nurse midwives (ANMs), accredited social health activists (ASHAs) and a male health worker responsible for comprehensive primary health care services for a population of about 5,000.
- Planning of health facility distribution in districts to ensure that a continuum of care is available on the principles of ‘time to care’ through a strong referral linkage.
- Digitization of family records and information from the community to the facility level.
- Use of real-time data to guide public health action and implementation monitoring.
- The HWCs would act as the ‘gateway’ for access to secondary and tertiary health services.
Enable mechanisms for rapid scale up
- Infusion of relevant work streams: Put in place the following work streams to create 150,000 well-functioning HWCs across the country –
- Infrastructure
- human resources (mid-level professional recruitment, training and deployment
- deployment and orientation of ANMs and male health workers)
- an Information and Communication Technology (ICT) system
- supply chain for drugs and disposables
- clinical and public health protocols and tools
- managerial/supervisory processes, and monitoring, evaluation and accountability systems
- Under Ayushman Bharat, put in place the necessary institutional mechanisms with a focus on health and wellness at the central and state levels for effective, timely and robust system level implementation as well as strong engagement with departments/directorates of health in the states.
- Establish special national and state level task forces and ‘command centres’.
- Create mechanisms for rapid scaling up of training.
- Develop empowered governance mechanisms for efficient decision-making, coordination, funds flow, procurement, contracting, recruitment, construction and implementation.
- Mobilize Corporate Social Responsibility (CSR) and Non-Resident Indians for funding HWCs.
- Some HWCs could also be mobile, particularly for better access to remote communities.
Coordinate action for disease prevention and public health promotion and to address social determinants of health
- Provide preventive services to improve healthy behaviours for family health and control the incidence of communicable and non- communicable diseases among the population covered by HWCs.
- Facilitate partnerships between HWC teams and other frontline development teams (nutrition, education, Swachh Bharat etc.) to engage with communities to address the socio-cultural and environmental determinants of ill health at the local level.
Catalyse people’s participation for healthy India: Swasth Bharat Jan Andolan
- Mandate and motivate HWC teams to work closely with village health, sanitation and nutrition societies, panchayati raj institutions as well as all other constituents of civil society in rural and urban spaces. This is vital because people are not just targets of health services but partners and multipliers of health-related activities.
Emphasise concurrent learning, operations research and innovation
- Undertake a well-funded research programme to find the best pathways for effective and context-specific scaling up of primary health care. This is critical because it is well-known that a single model of primary health care may not work for all districts/states in the country.
- Conduct research to assess the population-level health impact of the programme and effects on out-of-pocket expenses.
- Develop urban adaptations of comprehensive primary care.