The government’s efforts to provide better healthcare to people in rural areas seem to have resulted in improved utilization of the formal healthcare infrastructure.
Issue
Context
The government’s efforts to provide better healthcare to people in rural areas seem to have resulted in improved utilization of the formal healthcare infrastructure.
Background
- In India, healthcare is divided into two segments - public and private. The public healthcare segment is responsible for maintaining the primary health requirements in rural and urban areas and is funded by the government. The private healthcare segment in India is mainly focused in urban centres.
- The healthcare market is expected to increase about three-fold by 2022 and result in 8.6 trillion. This growth is to be augmented by a surge of 20-25% in the medical tourism sector in India. The number of medical tourist arrivals in India increased to 1.07 million in 2018 from 0.98 million 2017.
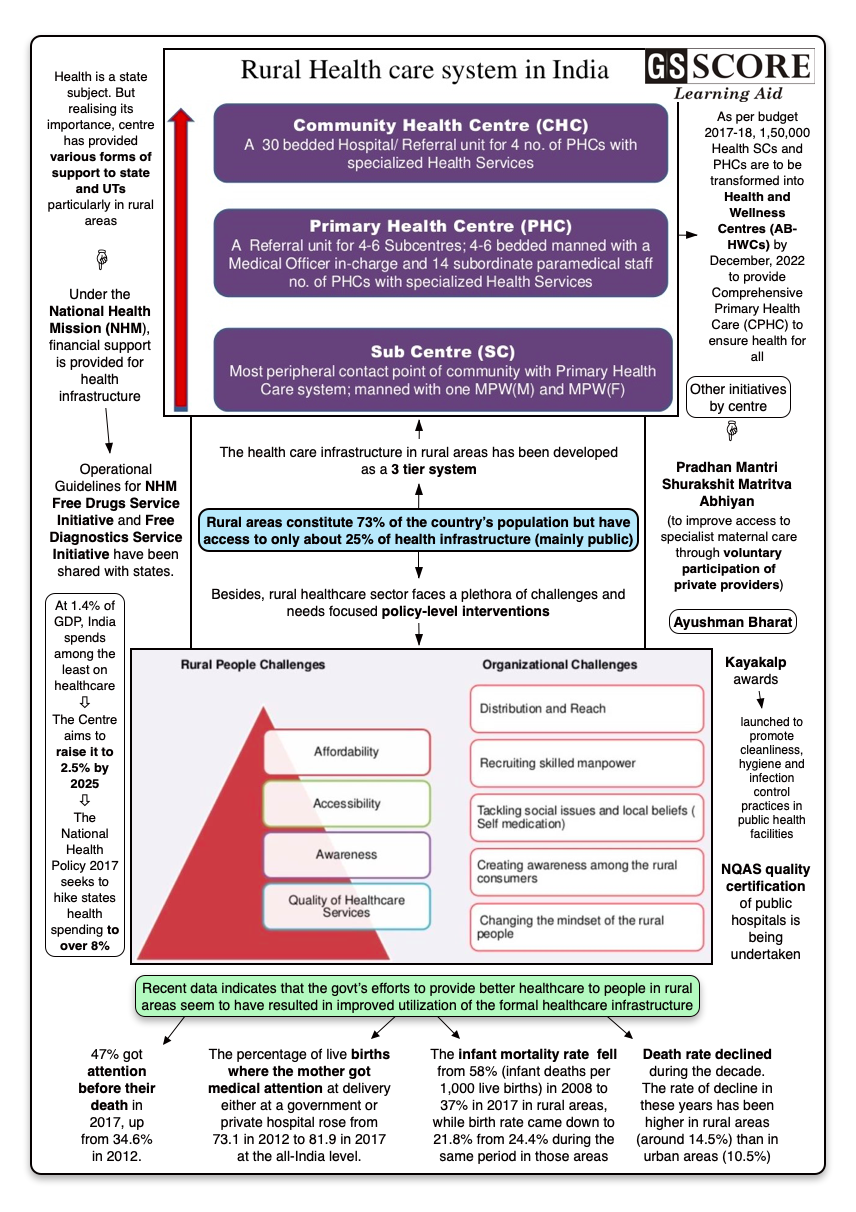
- However, the rural healthcare sector still faces a plethora of challenges and needs focused policy-level interventions.
- In India, 75% of the healthcare infrastructure is concentrated in urban areas where only 27% of the total Indian population is living. The remaining 73% of the country’s population is lacking proper primary healthcare facilities.
Rural Healthcare
Rural Health Care services in India are mainly based on Primary health care, which envisages attainment of healthy status for all. Also being holistic in nature it aims to provide preventive, promote curative and rehabilitative care services.
The health care infrastructure in rural areas has been developed as a three tier system as follows.
- Sub Centre: Most peripheral contact point between Primary Health Care System & Community manned with one Health Worker (Female)/ Auxiliary Nurse Midwife (ANM) & one Health Worker (M). The Sub Centre is the most peripheral and first contact point between the primary health care system and the community
- Primary Health Centre (PHC): A Referral Unit for 6 Sub Centres 4-6 bedded manned with a Medical Officer Incharge and 14 subordinate paramedical staff.
- Community Health Centre (CHC): A 30 bedded Hospital/Referral Unit for 4 PHCs with Specialized services
The situation of rural health care in India has not changed much during the past decade, though it is difficult to gauge from it from outside. The patients are still in the hands of quacks and unscientific medical practices. The villagers have to travel a long distances to the nearest hospital in case of emergencies and their only viable transportation is private transport which many cannot afford.
Shortcomings
Most people in rural India opt for government healthcare facilities because of monetary issues and as transport options to the urban centres are not very affordable. Despite that
- Only 11% sub-centres, 13% Primary Health Centres (PHCs) and 16% Community Health Centres (CHCs) in rural India meet the Indian Public Health Standards (IPHS).
- Only one allopathic doctor is available for every 10,000 people and one state run hospital is available for 90,000 people.
- Innocent and illiterate patients or their relatives are exploited and they are allowed to know their rights.
- Most of the centres are run by unskilled or semi-skilled paramedics and doctor in the rural setup is rarely available.
- Patients when in emergency sent to the tertiary care hospital where they get more confused and get easily cheated by a group of health workers and middlemen.
- Non-availability of basic drugs is a persistent problem of India’s rural healthcare.
- In many rural hospitals, the number of nurses is much less than required.
Other Constraints
Infrastructure
- The biggest concern for the rural healthcare system is the lack adequate infrastructure.
- The existing healthcare centres in rural areas are under-financed, uses below quality equipment, are low in supply of medicines and lacks qualified and dedicated human resources.
- Underdeveloped roads, railway systems, poor power supply are some of the major disadvantages that make it difficult to set up a rural healthcare facility.
Doctor
- Patient and Nurse-Doctor Ratio - Both these ratios contribute collectively to the inadequacy of the rural healthcare system.
- Every doctor needs a nurse to cater to their patients.
- The rural healthcare infrastructure is three-tiered and includes a sub-centre, a PHC and a CHC. PHCs are short of more than 3,000 doctors, with the shortage up by 200% over the last 10 years to 27,421 as per a report by India Spend.
- A patient is not always treated on time in rural India since the doctors are less in number.
Insurance
- Insurance is something that is severely lacking in rural healthcare.
- India has one of the lowest per capita healthcare expenditures in the world.
- The government has only contributed to about 32% for the insurance in healthcare sector in India which is sufficient.
Affordability
- People cannot afford the upmarket health services when they need to visit private hospitals.
- Advance technological advancements have also made healthcare costly.
- The cost of diagnostic facilities is also going up.
- Along with that, there are commissioned charges that most people don’t understand.
Lack of Awareness
- Awareness about proper healthcare is insufficient in India.
- Proper education on basic issues like the importance of sanitation, health, nutrition, hygiene and on healthcare policies, importance of medical services, their rights, financial support options, the need for proper waste disposal facilities.
- It is very important to inculcate a health seeking behaviour in them.
Lack of Medical Stores
- Medicines are often unavailable in rural areas.
- Supply of basic medicine is irregular in rural areas.
- The fair price shops (PPP model) are located in tertiary care and secondary care hospitals. These fair price shops charge differently in different locations.
- Discounts vary from 50% to 70% by the same provider on the same medicine.
Central Government Interventions
Public health being a State subject, the primary responsibility to provide improved access to healthcare services is that of the State Governments.
However, Central government provides financial and technical support to States and UTs to supplement their efforts for improving the healthcare services, particularly in rural areas via following initiatives –
- Under the National Health Mission (NHM), financial support is provided in the following areas: ASHAs workers, ambulances, mobile medical units (MMUs), drugs and equipments, support for Reproductive, Maternal, New-born, Child & Adolescent Health (RMNCH+A).
- As per the budget announcement 2017-18, 1,50,000 Health Sub Centres and Primary Health Centres are to be transformed into Health and Wellness Centres (AB-HWCs) by December, 2022 to provide Comprehensive Primary Health Care (CPHC) to ensure health for all.
- Operational Guidelines for NHM Free Drugs Service Initiative and Free Diagnostics Service Initiative have been shared with states. The objective is to ensure availability of essential drugs and necessary diagnostic services free of cost in public health facilities.
- Bridge Programme in Community Health - for Nurses and for Ayurveda Practitioners have been finalized. The trained personnel will provide comprehensive promotive and preventive and curative healthcare services.
- Kayakalp awards have been launched to promote cleanliness, hygiene and infection control practices in public health facilities. Additionally, NQAS quality certification of public hospitals is being undertaken.
- Pradhan Mantri Shurakshit Matritva Abhiyan (to improve access to specialist maternal care through voluntary participation of private providers).
- Ayushman Bharat
These central government initiatives over the past years to provide better healthcare to people in rural areas seem to have resulted in them tapping the formal healthcare infrastructure more.
Current Rural Healthcare Situation
- Latest data on live births, infant mortality and deaths suggests more people in rural areas are visiting doctors than ever before at private and government clinics/hospitals.
- The percentage of live births where the mother got medical attention at delivery either at a government or private hospital rose from 73.1 in 2012 to 81.9 in 2017 at the all-India level.
- 47% got attention before their death in 2017, up from 34.6% in 2012.
Best Performing States
- Nagaland fares the best with the lowest death rate and the lowest birth rate.
- The death rate in 29 states and Delhi for 2017 ranges from 3.6% in Nagaland to 7.5% in Chhattisgarh.
- Nagaland scores well on birth rates, too, sharing the fifth spot with Chandigarh at 13.5%
- The health indicators of its rural areas are good as well, with the birth rate at 14% against an all-India rural average of 21.8% and the death rate at 4.2% versus 6.9%.
- The IMR in its rural areas is 7%.
Percentage of GDP spent on healthcare
- At 1.4% of GDP, India spends among the least on healthcare.
- The Centre aims to raise it to 2.5% by 2025.
- The National Health Policy 2017 seeks to hike states health spending to over 8%.
Effect of better healthcare services on rural lives
- Fewer children are dying at birth not just in urban areas but also in rural regions.
- The infant mortality rate fell from 58% (infant deaths per 1,000 live births) in 2008 to 37% in 2017 in rural areas, while birth rate came down to 21.8% from 24.4% during the same period in those areas.
- Death rate declined during the decade. The rate of decline in these years has been higher in rural areas (around 14.5%) than in urban areas (10.5%).
Way Forward
Government has recognized that if basic healthcare does not reach the rural areas, no matter how much progress is achieved in the urban and semi-urban areas, the overall growth as a nation will be retarded.
Thus the Centre has made an outlay of ?64,999 crore for health in FY20, 16% higher than the FY19 revised estimates. Of this, ?33,651 crore is set aside for the government’s flagship scheme, the National Health Mission. It is an umbrella plan that now counts Ayushman Bharat, the world’s largest healthcare scheme, as its core plan to make medical care affordable for all.
Apart from these it should be ensured that –
- Affordable medical facilities are provided to people living in rural areas.
- Medical colleges need to encourage students to visit rural areas and understand the healthcare requirements of poor and downtrodden.
- Doctor in the government service must mandatorily serve in rural areas before getting his/her first promotion.
- Young doctors at grass roots level need to be sensitive to patients and their family.
- Private sector need to work with a spirit of altruism, commitment and missionary zeal in providing modern and affordable healthcare facilities in the rural areas and bridge the urban- rural divide.
- Medical associations should campaign to educate people on preventing lifestyle diseases which are slowly penetrating even the rural areas.
Learning Aid
Practice Question:
Enumerate the various initiatives taken by the government to augment rural health care in the country and examine how far they have been successful in tapping the formal healthcare infrastructure more. Also, suggest further interventions needed to provide them quality care.