
Alternative medical systems are entire systems of health theory and practice (including traditional Chinese medicine, Ayurvedic medicine, naturopathy, and homeopathy) that developed separately from conventional medicine. These systems typically use a variety of methods that fall under the CAM umbrella.
The Ministry of Ayurveda, Yoga, Naturopathy, Unani, Siddha, Sowa-Rigpa and Homoeopathy (abbreviated as AYUSH) is purposed with developing education, research and propagation of indigenous alternative medicine systems in India. Ministry of AYUSH (Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homoeopathy), will now be known as the Ministry of Ayush. The Ministry of Ayush includes the seven traditional systems of healthcare.
In 2016, World Health Organisation (WHO) published an eye-opening account of the incompetent health workforce of India based on the 2001 Indian census. According to WHO, the ideal doctor-patient ratio is 1:1000, whereas in India it is 1:1674. Furthermore, the report highlights the poor educational and medical background of the healthcare professionals in India - in allopathy, only 31.4% of allopathic doctors are educated up to the secondary level, and around 57.3% among them did not have any medical eligibility. In urban areas, only 58.4% of allopathic doctors had a valid medical qualification and this percentage was as low as 18.8% in the rural areas.
According to the Medical Council of India (MCI), the total number of medical practitioners in India was 9.32 lakh (as of September 30, 2014). However, the number of AYUSH doctors practising traditional medicine in the country is around 6.8 lakh, which is quite impressive.
he National Rural Health Mission (now known as National Health Mission) has recommended to mainstream the AYUSH system of indigenous medicine. Mainstreaming basically refers to the process of integrating AYUSH system of medicine with the existing health system in the country, at all levels of health care so that preventive, promotive and rehabilitative health care services can be offered to all sections of society.
he National Health Policy (NHP), 2017 has strongly advocated mainstreaming the potential of AYUSH within a pluralistic system of Integrative healthcare. The NHP, 2017 uses a new language of ‘medical pluralism’ and reemphasizes the need for integrating AYUSH in the National Health Mission, research and education
integrating AYUSH with accredited social health activists (ASHA) workers by training them on relevant aspects of AYUSH; implementing initiatives for ensuring availability of AYUSH drugs at all levels; strengthening quality control mechanism in laboratories to avoid manufacture and sale of counterfeit and substandard drugs
Launch of e- AUSHADHI portal by Ministry of AYUSH is the landmark for promoting and consolidation of alternative medicine system in India as it helps in licensing of ayurveda, siddha, unani, and homeopathy drugs and related matters and also maintain transparency, improved information management facility and data usability.
The 4th Common Review Mission Report, 2010 of the National Health Mission, brought to light a significant find - various states across India including Assam, Chhattisgarh, Maharashtra, Madhya Pradesh and Uttarakhand had deployed AYUSH practitioners as medical officers in public health centres (PHCs). In the present times, the fundamental aspects of holistic systems are not appropriately positioned in most of the clinical trials designed to examine the safety and efficacy of AYUSH therapies/ approaches.
- ,The first National Health Policy of India (NHP) got formulated only in 1983 with its main focus on provision of primary health care to all by 2000, prioritized setting up a network of primary health care services using health volunteers and simple technologies
- NHP 2002 was brought on the basis of NHP 1983 with an objective of providing health services to general public through decentralisation, use of private sector and increasing expenditure of public health care. Also emphasised on the use of Non-Allopathic form of medicines.
- India’s health system has been divided between state and central government, where the Union Ministry of health and Family welfare is the nodal agency for effective implementation of public health care in India followed by state governments to adapt.
- Union ministry role: prevention and control of major communicable diseases, and promotion of traditional and indigenous systems of medicines and setting standards and guidelines,
- State government role: the areas of public health, hospitals, sanitation and so on come under the purview of the state, making health a state subject.
- However, areas having wider ramification at the national level, such as family welfare and population control, medical education, prevention of food adulteration, quality control in manufacture of drugs, are governed jointly by the union and the state government.
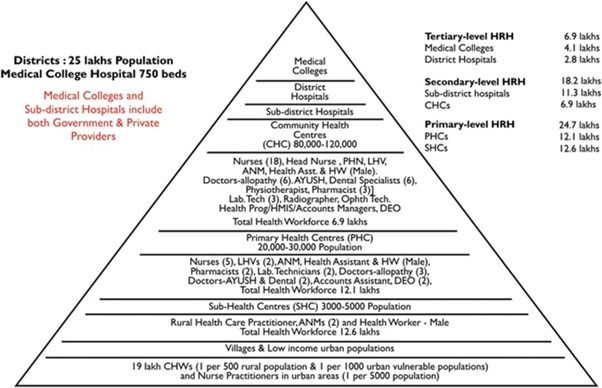
- Structure of Public health-care infrastructure:
The public health-care infrastructure in rural areas has been developed as a three-tier system based on the population norms. It includes:
- Sub-centre; established in an area with population of 5000 and in hilly area with a population of 3000.
- Primary health centres; In plain area with population of 30000 and in hilly area with a population of 20000 and is the first contact between village community and medical officer.
- Community health centres; is established by state government where people is around 1,20,000 in plain area and 80,000 in hilly area.
- First referral units; An existing facility (district hospital, sub-divisional hospital, CHC) can be declared a fully operational first referral unit (FRU) only if it is equipped to provide round-the-clock services for emergency obstetric and newborn care, in addition to all emergencies that any hospital is required to provide. It should be noted that there are three critical determinants of a facility being declared as a FRU: (i) emergency obstetric care including surgical interventions such as caesarean sections; (ii) care for small and sick newborns; and (iii) blood storage facility on a 24-h basis.
In health sector, India has made enormous strides over the past decades. The life expectancy has crossed 67 years, infant and under-five mortality rates are declining as is the rate of disease incidence. Many diseases, such as polio, guinea worm disease, yaws, and tetanus, have been eradicated.
- The Maternal Mortality Ratio (MMR) of Indiahas declined by 10 points as per a special bulletin released by the Registrar General of India. It has declined from 113 in 2016-18 to 103 in 2017-19 (8.8 % decline). The country had been witnessing a progressive reduction in the MMR from 130 in 2014-2016, 122 in 2015-17, 113 in 2016-18, and to 103 in 2017-19.
- The life expectancy at birth in 2019 was 69.5 years for men and 72 years for women, which came down to 67.5 years and 69.8 years, respectively, in 2020
- The infant mortality rate for India in 2021 was 28.771 deaths per 1000 live births, a 3.61% decline from 2020. The infant mortality rate for India in 2020 was 29.848 deaths per 1000 live births, a 3.48% decline from 2019.
- There is a massive shortage of medical staff, infrastructure and last mile connectivity in rural areas Doctor: Population 1:1800 and 78% doctors cater to urban India (population of 30%).
- Doctor: Population 1:1800 and 78% doctors cater to urban India (population of 30%).
- There is a shortage of PHCs (22%) and sub-health centres (20%), while only 7% sub-health centres and 12% primary health centres meet Indian Public Health Standards (IPHS) norms.
- India’s expenditure on the health sector has risen meagerly from 1.2 per cent of the GDP in 2013-14 to4 per cent in 2017-18. The National Health Policy 2017 had aimed for this to be 2.5% of GDP.
- Reducing side effects as they depend upon various Natural way methods over chemical/lab made medicine.
- More control over health condition.
- Encourages feelings of well-being, pleasure, positivity.
- Cost effective compared to conventional medicine.
- Reliable as they have minimal side effects.
- Helps in time of post surgery or post conventional treatment for rehabilitation.
- Helps in reducing excessive load on hospitals and support in achieving more efficiency in public health care system.
- Creates more opportunities to students in medical science arena, If more importance and awareness generated.
- Country’s medical tourism has more scope to grow more.( India is ranked 10th out of the top 46 countries in the world in the Medical Tourism Index 2020-21 by Medical Tourism Association.) Resulting in growth of foreign tourist arrival (FTA).
- All these can lead to exponential growth of alternative medicine in Indian and has scope in reducing the cost of conventional treatment charges enabling more efficient public-health care eco system in India.
- Has minimal scientific research, resulting less foot fall in such hospitals.
- As their treatment procedures not suitable for emergency cases, they won’t be best options in time of emergency.
- Takes more time to get benefits of treatment, Resulting loss of interest in patients and family members.
- Less regulation compared to conventional medicine.
- Diagnosis can be the main issue in determining patient’s health condition.
- Limited coverage/acceptance by health insurance companies
- Even use of herbs and natural methods of treatment, some reactions may worsen the situation.
- Concern with fake practitioners.
The alternative medicine system in recent time shown up ample amount of growth due to its advantages, not only in India but also in many other countries
- The WHO estimates that 70–90% of the rural population in developing countries use HM to meet, in part or completely, their health
- A NSSO survey in 2014 found that only 6.9% of the population favoured AYUSH (3.5% ISM and 3.0% homeopathy) over conventional mainstream medicine
- A 2014 study did not report any significant difference between the usage of AYUSH services by rural and urban populace, after adjusting for socioeconomic and demographic variables
- The treatments were more used among females in rural India but no gender-differential was observed in the urban populations. Chhattisgarh (15.4%), Kerala (13.7%), and West Bengal (11.6%) displayed the highest AYUSH utilization levels.
- There is no credible efficacy or scientific basis of any of these forms of treatment
- As of March 2015, there were nearly 800,000 AYUSH practitioners, over 90 per cent of whom practiced homeopathy or ayurveda.
- A 2018 study by the Confederation of Indian Industry (CII) estimated the market share of AYUSH medicines at around US$3 billion and that India exported AYUSH products of a net worth US$401.68 million in the fiscal year 2016–17.
- The Department of Pharmaceuticals had allocated a budget of ₹1.44bn to the ministry for 2018-2020 for manufacture of alternative medicines.
- The AYUSH ministry collaborated with CSIR( Council for Scientific and Industrial Research) to setup Traditional Knowledge Digital Library in 2001 which includes Ayurveda, Unani, Siddha and Yoga to counter bio piracy.
The role of Alternative medicine system in public health is inevitable to an extent but some limitations were also applicable due to their disadvantages and given unproven/ limited scientific data which raise major concern. But the statistical data provides that people in recent days resorting to natural and herbal medicinal system to avoid conventional medicine and their side effects. This shows a positive side in alternative medicine system. Institutional support such as R&D, more financial and infrastructural assistance along with awareness can help out alternative medicine to best suitable for public health.
Related Articles


